JAW LOCK (TMJ)

Have a locked jaw?
Let’s address the following questions
with Dr. Tetri:
Why does the jaw lock?
How dangerous is it?
What should you do before seeing a doctor?
What diagnostic and treatment methods are used for a locked jaw?
What is a jaw lock?
Jaw lock is a condition where the movement of the lower jaw is severely restricted due to a spasm of the jaw muscles (internal pterygoid, masseter, temporalis). It locks in one of the positions — either open or closed. Your speech and the ability to swallow become impaired, and breathing becomes difficult.
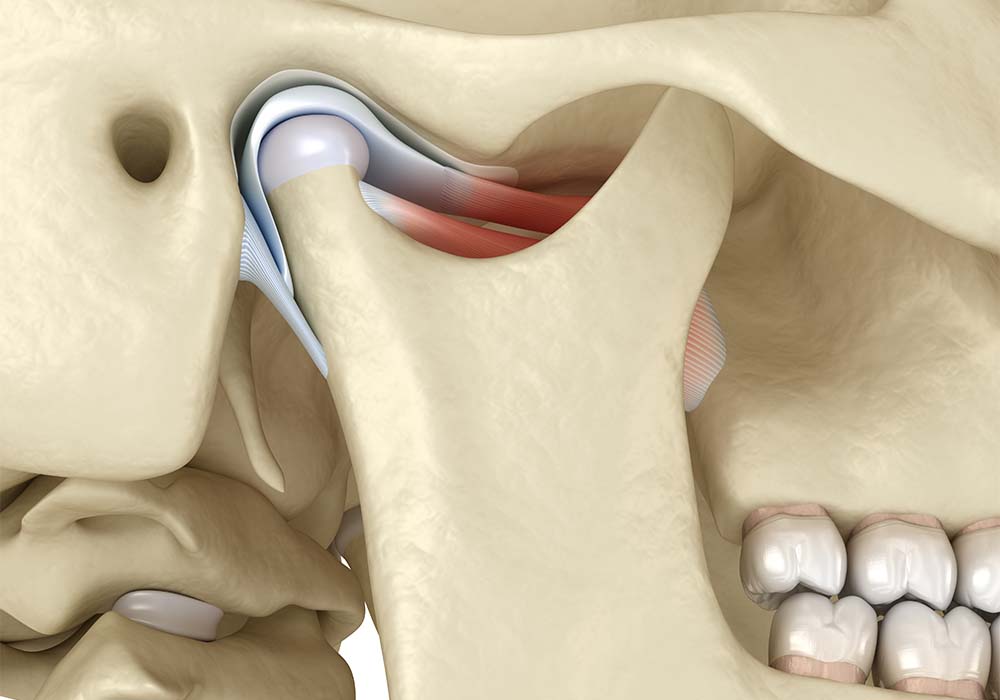
The temporomandibular joint (TMJ) is a paired anatomical entity that provides horizontal/vertical movement of the lower jaw relative to the upper jaw. The jaw mobility is provided by the joint and the chewing muscles of the face, controlling these movements. If they are damaged, the jaw becomes locked.
Symptoms of a locked jaw
- Crunching/clicking when opening or closing the mouth
- Constant feeling of tension in the facial muscles
- Pain in the ear area even at rest
- Limited closing of the jaw
- Asymmetrical opening of the mouth.
- Profuse salivation
- Swallowing problems
- Slurred speech or complete inability to open the mouth
- Change in the facial symmetry
- Prolapse/retraction of the lower jaw
- Strong clenching of the teeth
- Sometimes the body temperature goes up.
Causes of a jaw lock
Forms
Depending on the degree of mouth opening restriction, there are three forms of trismus:
Types
How to unlock the jaw: What can be done?
Before visiting a doctor, you can alternately apply a warm and a cold compress to the sore joint once every hour for 5-10 minutes. You can apply cream to relax the spastic muscles during a break. This will help to relieve the condition slightly and possibly unlock the jaw.
If the jaw keeps locking, you can try relaxing the chewing muscles with finger massage, applying medium force.
You can take an over-the-counter painkiller from your medicine cabinet to relieve pain.

Jaw stuck: Should I see a doctor?
At the first symptoms, see a doctor. It is necessary to treat the TMJ dysfunction immediately. Do not self-medicate and bring the situation to a critical state when the mouth will not open/close at all.
Given the relationship between occlusal pathologies and temporomandibular joint dysfunction, TMJ dysfunction should be treated by a physician with gneuromuscular dentistry skills.

Diagnosis
A CT scan allows for a qualitative examination of the maxillofacial area. It shows the:
- Position of the articular disk
- Damage level of the epiarticular soft tissues
- Abnormalities of the articular disk
- Thickness and structure of the masticatory muscles
- Changes in the shape and size of articular surfaces of the TMJ, etc.
Special sensors are attached to the patient’s face (from the temporal lobe to the mandibular joint) to calculate the compression strength of the masticatory muscles. The sensors are extremely sensitive, with data accuracy up to 20 microns, and detect even the slightest deviations from the correct occlusion.
This is a technique for obtaining an objective characteristic of the TMJ pathology and analyzing the relationship of the articular disk with the articular head, based on a noise recording during several cycles of mouth opening and closing.
Jaw lock: GNM treatment
There is no sole treatment plan — it is different with each individual, and depends on the clinical situation. A combination of the following methods is used:
An occlusal splint is placed on the patient’s teeth:
- It forces the articular heads to the correct position
- It regulates the activity of the facial muscles
- It helps to stretch the shortened ligaments
- It fixes the jaw in an anatomically correct position.
Transcutaneous Electrical Nerve Stimulation is ultra-low-frequency electromyostimulation of the masticatory muscles, which relieves their spasm and restores elasticity. After “resetting”, the facial muscles return to the physiologically correct position. The lower jaw and temporomandibular joints return to place.
Orthodontic treatment with braces or aligners can be performed after normalization of the TMJ function.
Ideally, you should plan the bite correction process in a special program before treatment begins. An intraoral scanner takes digital impressions, then they are loaded into the program, and after that a 3D model of the correct bite is projected.
Preventing jaw lock
- It is necessary to have preventive check-ups at the dentist every 4 months
- To timely treat dental diseases and risk factors for the development of TMJ dysfunction (neurological diseases, bruxism, etc.)
- To correct bite anomalies in time
- To periodically undergo tone correction of the masticatory muscles
- If teeth are missing, they can be restored with dentures on implants.
Schedule a consultation with Dr. Tetri to find out the reason why your jaw is locked, and what you need to do to get it working properly again!

